This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
,
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Blog Layout
Post Title
June 17, 2020
Suffering from Sensitive Teeth?
Is the taste of ice cream or a sip of hot coffee sometimes a painful experience for you? Does brushing or flossing make you wince occasionally? If so, you may have sensitive teeth.
However, you’re not alone. As a matter of fact, statistics show that 1 out of 8 American adults suffer from sensitive teeth.
Possible causes include:
• Tooth decay (cavities)
• Fractured teeth
• Worn fillings
• Gum disease
• Worn tooth enamel
• Exposed tooth root
In healthy teeth, a layer of enamel protects the crowns of your teeth—the part above the gum line. Under the gum a layer called cementum protects the tooth root. Underneath both the enamel and the cementum is dentin.
Dentin is less dense than enamel and cementum and contains microscopic tubules (small hollow tubes or canals). When dentin loses its protective covering of enamel or cementum, these tubules allow heat, cold, acidic or sticky foods to reach the nerves and cells inside the tooth. Dentin may also be exposed when gums recede. The result can be hypersensitivity.
Sensitive teeth can be treated. The type of treatment will depend on what is causing the sensitivity. Since tooth sensitivity is an uncomfortable situation that limits your ability to enjoy certain foods, it is better to get it checked out sooner rather than later.
Upon having a discussion to understand more about your teeth sensitivity, Dr. Chubb may suggest one of a variety of treatments:
• Desensitizing toothpaste.
This contains compounds that help block transmission of sensation from the tooth surface to the nerve, and usually requires several applications before the sensitivity is reduced.
• Fluoride gel.
An in-office technique which strengthens tooth enamel and reduces the transmission of sensations.
• A crown, inlay or bonding.
These may be used to correct a flaw or decay that results in sensitivity.
• Surgical gum graft.
If gum tissue has been lost from the root, this will protect the root and reduce sensitivity.
• Root canal.
If sensitivity is severe and persistent and cannot be treated by other means, your dentist may recommend this treatment to eliminate the problem.
Proper oral hygiene is the key to preventing sensitive-tooth pain. Our Amazing Smiles
staff is here to answer questions you may have about your daily oral hygiene routine or concerns about tooth sensitivity.

By 7001124384
•
February 19, 2024
Clenching or grinding your teeth while you're asleep is pretty common among children and adults. But when it starts to cause headaches, tooth or jaw pain, or damage to your teeth, it's time to talk to your dentist about bruxism. A common treatment for sleep bruxism is a night guard. Learn more about sleep bruxism and night guards to protect your teeth. Maybe this has happened to you: you wake up and immediately feel a headache. Or, you've noticed your jaw is a little sore, or perhaps you've even had chipped or lose teeth. These are common signs of bruxism—or teeth grinding. Thankfully, your dentist and dental hygienist are trained to look for signs of bruxism and help you with treatment. They may recommend a mouthguard to wear at night, an easy way to protect your teeth from damage from grinding and clenching. Nightguards have many names. They are also called mouthguards, occlusal guards, dental guards, bite splints, or nocturnal bite plates. They are retainer-like soft or hard plastic pieces that cover either the top or bottom set of teeth. Nightguards are popular treatments for sleep bruxism. Nightguards cushion your teeth from the force of clenching and prevent the teeth from grinding together, preventing headaches, damaged teeth, and inflamed gums. Learn about sleep bruxism and its characteristic signs and symptoms, and the popular forms of treatment recommended by dentists, including night guards. What is Sleep Bruxism? If you frequently wake up with a headache, tooth, or jaw pain, you may want to ask your dental hygienist if you have bruxism. According to the American Academy of Oral Medicine, teeth grinding is common among children and adults at times. Still, if it's frequent enough to cause issues with your teeth or jaw, it's time to speak to a dental professional. Common Signs of Sleep Bruxism Talk to your dentist about the following signs and symptoms: Chipped teeth Waking up with headaches Temporomandibular Joint Disorder—inflammation of the jaw due to clenching Taking antidepressants with paroxetine Chronic grinding Sleep Bruxism in Children It is common for children to grind their teeth at some point, especially children under five. Most children outgrow teeth grinding without treatment, with no harm to their teeth. Still, your dentist may recommend treatment depending on the severity of the bruxism. Nightguards There are several ways to reduce the impact of bruxism on your oral health. One of the most common is a night guard: a mouthguard typically worn while sleeping. Some night guards are available without a prescription at most pharmacies. To use it, you boil it or microwave it (follow instructions), let it cool for a few seconds, and then gently bite it to shape it to your mouth. Customized Night Guards from Your Dentist Nightguards are also available from your dentist. Customized guards tend to be of a higher quality and are custom-made to your teeth. Your dentist will take an impression of your teeth, then send the resulting mold to a dental laboratory. This facility will create a custom-fitted night mouthguard for you. Your dentist will check the mouth guard's fit and make any necessary adjustments before you take it home. Typically a customized night guard is a more expensive device than ones purchased over-the-counter. Still, it can be more comfortable to wear. Caring for Your Mouthguard It's best to put the mouthguard in just before sleeping. You can take it out as soon as you wake up. It should start feeling comfortable after wearing it for four to six weeks. According to the Cleveland Clinic, you should wash your guard before and after each use. Rinse your mouthguard with clean, cold water or brush it with a toothbrush and toothpaste. Don't leave the night guard in a sunny spot or hot area. Don't wash it with hot water either, because the plastic could warp and no longer fit you properly. Store your mouthguard in a container and check it regularly. If you find that your guard feels loose or uncomfortable, it's probably time to replace it. Other Treatments for Teeth Grinding If a night guard is uncomfortable, you can talk to your dentist about other treatment options: Stress prevention: One of the leading causes of bruxism is anxiety. Taking time to unwind before bed can reduce your teeth clenching and grinding. You can read a book, do a bedtime yoga routine, or take a warm bath. Keep a sleep log: A sleep log or diary includes when you went to bed when you woke up, and any time you were up during the night. Spending a few minutes in the evening and morning to reflect on sleep quality will help identify what may contribute to bruxism. Change of diet or medication: Your dentist might recommend avoiding stimulants like caffeine because that can increase teeth grinding. Certain medications, like antidepressants, might also contribute to the issue. So, tell your dentist about medications you are taking so they can suggest an alternative if one is warranted. The most important thing to know about bruxism is that it can be treated with your dental hygienist and dentist's help. If you are experiencing pain or discomfort, you are not far away from finding relief.

By 7001124384
•
February 14, 2024
Why should I replace missing teeth? Your appearance is one reason. Another is that the gap left by a missing tooth can mean more strain is put on the teeth at either side. A gap can also mean your ‘bite' is affected, because the teeth next to the space can lean into the gap and change the way the upper and lower teeth bite together. This can then lead to food getting packed into the gap, which causes tooth decay and gum disease. How are missing teeth replaced? This depends on the number of teeth missing and on where they are in your mouth. The condition of the teeth you still have also affects the decision. There are three main ways to replace missing teeth. The first is with a removable false tooth (or teeth) - called a partial denture. The second is with a fixed bridge. A bridge is usually used when there are fewer teeth to replace, or when the missing teeth are only on one side of the mouth. The third way is by the use of dental ‘implants'. This is where an artificial root is placed into the bone of the jaw and a crown or bridge placed on top of this. See our leaflet ‘Tell me about: dental implants'. What is a partial denture? This is a plate with one or more false teeth on it. It may be all plastic or a mixture of metal and plastic. Both types may have clips (clasps) to help keep the denture in place in your mouth. Depending on where they are, some of these clips may show when you smile or open your mouth. What is the difference between a plastic partial denture and one that contains metal? Plastic partial dentures are less expensive to make. But unless they are designed very carefully they can damage the teeth they fit against. Metal partial dentures are usually made from an alloy of cobalt and chromium, and they are much stronger. They are lighter to wear and can be supported by the remaining teeth. Although the base is metal, they have gum-coloured plastic and natural-looking teeth fixed to them. They are more expensive than plastic ones. How do I choose the best type for me? Be guided by your dentist. They will know the condition of your remaining teeth. In most cases a metal-based partial denture gives the best result. Can I have a bridge fitted straight after having a tooth removed? It can take up to 6 months for your gums to heal properly after an extraction. This means that you may need to have a temporary denture before the bridge is fitted. How do I look after my denture? Dentures may break if you drop them. Always clean your denture over a bowl of water or a folded towel in case you drop it. To clean your dentures, the general rule is: brush and soak every day. Brush your dentures first, to help remove any bits of food. Use a non-abrasive denture cleaner, not toothpaste. Be careful not to scrub too hard as this may cause grooves in the surface. Make sure you brush all the surfaces of the dentures, including the surface that fits against your gums. This is especially important if you use any kind of denture fixative. Soak your dentures every day in a denture-cleaning solution. This will help remove any plaque and stubborn stains that are left. It will also help to disinfect your dentures, leaving them feeling fresher. Always follow the manufacturer's instructions. Don't keep your dentures in overnight unless there are specific reasons for you to keep them in. If you notice a build-up of stains or scale, have your denture cleaned by your dental team. Should I take my denture out at night? Your dental team may recommend taking out your dentures at night to give your mouth a chance to rest. If you do this, it is important to leave it in water to prevent any warping or cracking. What is the alternative to a partial denture? The main alternatives are a fixed bridge or a dental implant. A dental bridge is made by putting crowns on the teeth at either side of the gap, and then joining these two crowns together by placing a false tooth in the space. This is all made in the laboratory and then the pieces are cemented into place with special adhesives. The bridge can't be removed. Another option is an adhesive bridge. This has ‘wings' that are bonded to the back of the supporting teeth, with very little drilling needed. Can I always have a bridge to replace missing teeth? You can have a bridge only if you have enough strong teeth with good bone support. Your dental team will help you decide which is the best way of replacing missing teeth. What are bridges made of? Bridges are usually made of porcelain bonded to precious metal. Sometimes other non-precious metals are used in the base for strength. There are also new bridges made entirely of a special type of strong porcelain. What will a bridge cost? The cost will vary depending on the size and type of bridge you need. Always get a written estimate and treatment plan before starting any dental treatment. Although a bridge may seem expensive it should last many years. How do I look after my bridge? You need to clean your bridge every day, to prevent problems such as bad breath and gum disease. You also have to clean under the false tooth every day. Your dentist or hygienist will show you how to use a bridge needle or special floss, as a normal toothbrush cannot reach. Are there other methods for fixing false teeth? There are other methods, such as using a combination of crowns and partial dentures that can keep the retaining clips out of sight. These are quite specialised dentures, so you should ask your dental team about them. Can I have teeth which attach to the jawbone? Yes, by having implants. This treatment means you may be able to replace missing teeth without having crowns on other teeth. Click here for more information about dental implants. Remember that it is as important to care for your remaining teeth as it is to replace the missing ones. article provided by Oral Health Foundation

By 7001124384
•
January 31, 2024
Questions & Answers with Dr. Kimberly Chubb Why should I visit the dentist every six months for a routine exam and cleaning? An ounce of prevention is worth a pound of cure. Bacteria, food debris, and sugar can produce cavities in the grooves of your molars and in between all your teeth. We can detect these early with regular visits or help you avoid them with specific oral hygiene techniques. Preventive measures with fluoride, sealants, rinses, or dental appliances can fine tune your needs. We assess you as an individual wand work with you to personalize and optimize your dental health. What is a typical example you observe as a dentist when people don’t keep regular dental visits? A patient contacts our office regarding moderate to severe pain related to a dental abscess or gum abscess. Their dental emergency is usually a deep cavity into the nerve of a tooth or a gum abscess that has damaged the bone area around the roots of one or more teeth. Either problem results from bad bacteria that cause destruction and produce pus. The body then sends a signal to alert us of the problem in the form of pain. This alert should be respected. Some people try and tough out the pain, take pain pills or use ointment to disguise the pain. Over time, the pus continues to destroy the nerve in the area and the pain will subside, but the problem progresses undetected. This is the worst scenario. The infection can progress to tooth extraction or destruction to the jawbone. Chronic dental infections have clearly shown to spread throughout the body and can cause additional harmful problems to the heart and organs. Routine dental visits identify problems early and allow for corrective treatment before the problems reach a more advanced stage. How is Amazing Smiles a special dental office for new patients to consider? We always put our patients first and our track record speaks for itself. Patients have provided us with hundreds of 5-star reviews describing us as “considerate”, “knowledgeable”, “thorough”, “very professional” and many others. We are proud to achieve these accolades from our patients, and we work hard every day to ensure our patients are fully satisfied. Compassion and caring are the backbone to our practice, and we continually update the technology to remain state-of-the-art. Our staff is focused on you as a person, and it shows. We accept most insurances and have quality payment plan options. We welcome new patients to Amazing Smiles Family Dentistry and extend this same professional and caring approach to their dental health.
By 7001124384
•
January 16, 2024
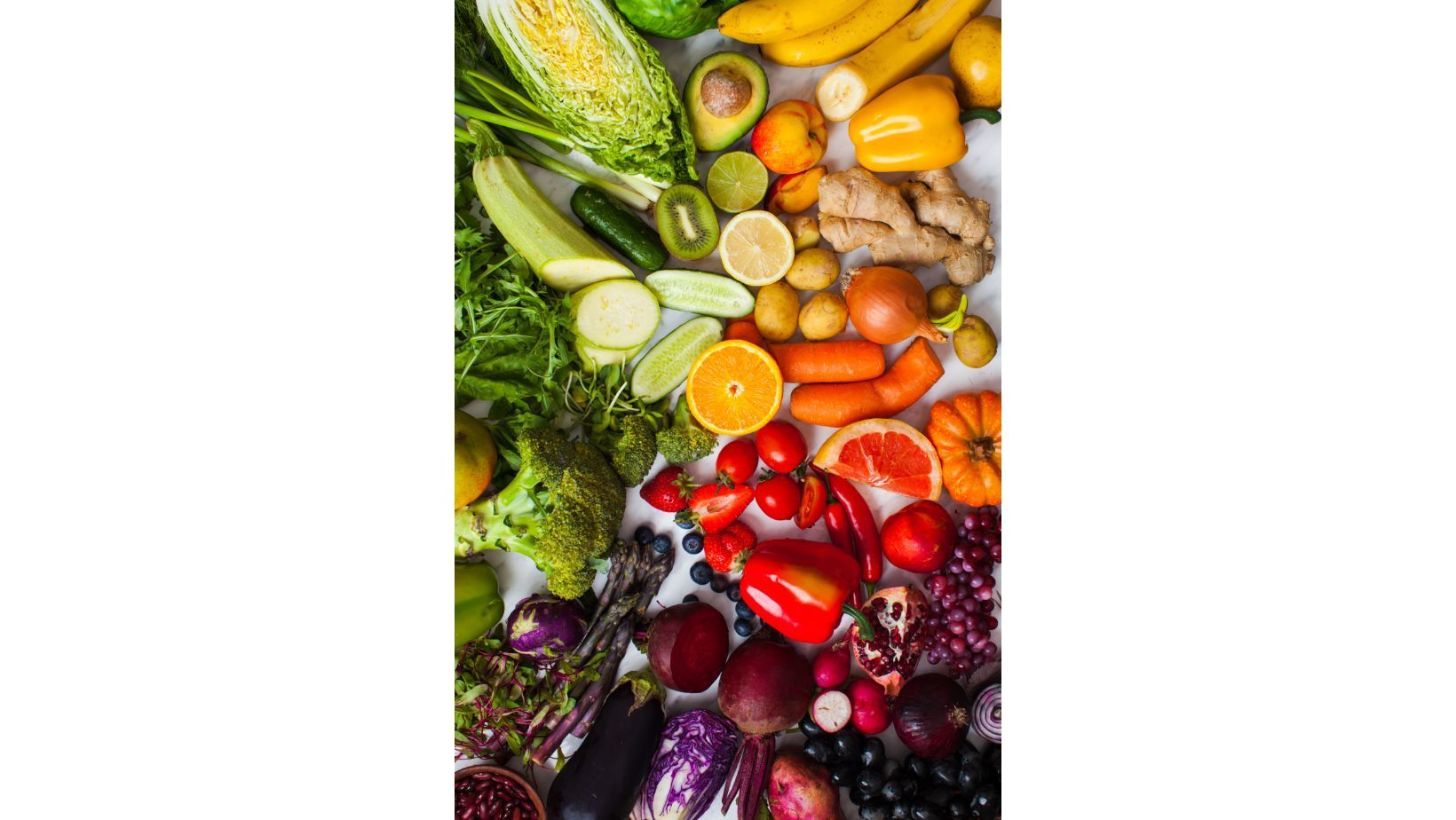
In recent years, the surge in popularity of veganism has sparked conversations about its impact on various aspects of health, including oral health. As more people adopt a plant-based lifestyle for ethical, environmental, or health reasons, it's essential to explore how this dietary choice influences our teeth and gums. In this blog, we'll delve into the relationship between vegan food and oral health, highlighting the potential benefits and considerations for maintaining a healthy smile on a plant-based diet. Nutrient-Rich Vegan Foods for Strong Teeth One of the key advantages of a vegan diet lies in its emphasis on nutrient-dense foods. Many plant-based options are rich in essential vitamins and minerals crucial for maintaining optimal oral health. Leafy greens, such as kale and spinach, provide calcium for strong teeth, while nuts and seeds offer phosphorus, a vital component for enamel strength. Additionally, fruits and vegetables high in vitamin C, like strawberries and bell peppers, contribute to healthy gums and collagen production. Alkaline Foods and Oral pH Balance Maintaining an optimal pH balance in the mouth is vital for preventing tooth decay and gum disease. Animal products and processed foods can often contribute to acidity in the body, potentially leading to an imbalance in oral pH. On the other hand, many plant-based foods, such as fruits, vegetables, and legumes, tend to be alkaline-forming. This can create a more favourable environment for oral health, helping to neutralize acids and promote a healthier balance. The Role of Antioxidants in Oral Health Vegan diets, abundant in colourful fruits and vegetables, provide an excellent source of antioxidants. Berries, green tea, and cruciferous vegetables are examples of antioxidant-rich foods that can benefit not only your overall health but also your oral wellbeing. Mindful Snacking and Tooth-Friendly Choices While vegan diets offer a plethora of tooth-friendly options, it's important to be mindful of certain snacks that may pose challenges to oral health. Dried fruits, for instance, can be high in natural sugars and may stick to teeth, therefore you should only eat them as part of a meal not snack on dried fruit in-between meals. Dried fruit stuck in the grooves of the teeth, has the potential to cause dental decay if not successfully removed. Opting for fresh fruits or raw vegetables as snacks, along with drinking water or using a fluoride mouthwash to rinse can help mitigate these concerns. Maintaining Proper Nutrient Balance While a vegan diet can be incredibly nutritious, it's essential to ensure a well-balanced intake of nutrients. Vitamin B12, iron, zinc, and omega-3 fatty acids are nutrients commonly found in animal products, and vegans may need to supplement or carefully plan their diet to meet these requirements. These nutrients play a crucial role in overall health, including oral health, so it's vital to address any potential deficiencies. Conclusion Embracing a vegan lifestyle can bring about numerous health benefits, including positive effects on oral health. By focusing on nutrient-dense, alkaline-forming foods and maintaining a well-balanced diet, individuals can nourish their smiles from the inside out. Written by Oral Health Foundation
By 7001124384
•
January 4, 2024
Dental Health and Dry Mouth We all need saliva to moisten and cleanse our mouths and digest food. Saliva also prevents infection by controlling bacteria and fungi in the mouth. When you don't make enough saliva, your mouth gets dry and uncomfortable. Fortunately, many treatments can help against dry mouth, also called xerostomia. What Causes Dry Mouth? Causes of dry mouth include: • Side effect of certain medications. Dry mouth is a common side effect of many prescription and nonprescription drugs, including drugs used to treat depression, anxiety, pain, allergies, and colds (antihistamines and decongestants), obesity, acne, epilepsy, hypertension (diuretics), diarrhea, nausea, psychotic disorders, urinary incontinence, asthma (certain bronchodilators), and Parkinson's disease. Dry mouth can also be a side effect of muscle relaxants and sedatives. • Side effect of certain diseases and infections. Dry mouth can be a side effect of medical conditions, including Sjögren's syndrome, HIV/AIDS, Alzheimer's disease, diabetes, anemia, cystic fibrosis, rheumatoid arthritis, hypertension, Parkinson's disease, stroke, and mumps. • Side effect of certain medical treatments. Damage to the salivary glands, the glands that make saliva, can reduce the amount of saliva produced. For example, the damage could stem from radiation to the head and neck, and chemotherapy treatments, for cancer. • Nerve damage. Dry mouth can be a result of nerve damage to the head and neck area from an injury or surgery. • Dehydration. Conditions that lead to dehydration, such as fever, excessive sweating, vomiting, diarrhea, blood loss, and burns can cause dry mouth. • Surgical removal of the salivary glands. • Lifestyle. Smoking or chewing tobacco can affect how much saliva you make and aggravate dry mouth. Breathing with your mouth open a lot can also contribute to the problem. What Are the Symptoms of Dry Mouth? Common symptoms include: • A sticky, dry feeling in the mouth • Frequent thirst • Sores in the mouth; sores or split skin at the corners of the mouth; cracked lips • A dry feeling in the throat • A burning or tingling sensation in the mouth and especially on the tongue • A dry, red, raw tongue • Problems speaking or trouble tasting, chewing, and swallowing • Hoarseness, dry nasal passages, sore throat • Bad breath Why Is Dry Mouth a Problem? Besides causing the symptoms mentioned above, dry mouth also raises your risk of gingivitis (gum disease), tooth decay, and mouth infections, such as thrush. Dry mouth can also make it hard to wear dentures. How Is Dry Mouth Treated? Treatment for dry mouth depends on what is causing the problem. Generally, treatment focuses on three areas: • Managing other medical conditions • Preventing tooth decay • Increasing the flow of saliva, if possible Managing Causes of Dry Mouth If you think your dry mouth is caused by certain medication you're taking, talk to your doctor. The doctor may adjust the dose you're taking or switch you to a drug that doesn't cause dry mouth. But if the medical condition causing the dry mouth can’t be changed -- for example, if the salivary gland has been damaged or is a result of a disease itself, as with things like Sjögren's syndrome, Alzheimer's disease, and stroke -- treatment will focus on ways to increase saliva flow. Preventing Tooth Decay Due to Dry Mouth Not only does saliva help digest food and make it possible for you to chew and swallow, it is the natural mouth cleanser. Without saliva, tooth decay and gum disease are more likely. If you have a dry mouth, to fight tooth decay and gum disease, you need to be extra careful about following good oral hygiene habits, which consist of: • Brushing your teeth at least twice a day (but preferably more often), after every meal and before bedtime • Flossing your teeth every day • Using a toothpaste that contains fluoride • Visiting your dentist for a checkup and cleaning at least twice a year; your dentist may recommend a daily fluoride rinse or fluoride gel to keep your teeth healthy. Increasing the Flow of Saliva With Dry Mouth If you have dry mouth, your doctor may also prescribe an oral rinse to restore mouth moisture. You can get these products over the counter in a rinse or spray. And there are toothpastes, mouthwashes, and moisturizing gels just for dry mouth; ask your dentist or doctor about them. If that doesn't help, they may prescribe a medication that boosts saliva production called Salagen. Another prescription drug, Evoxac, is FDA-approved to treat dry mouth in people with Sjögren's syndrome, an autoimmune disease linked to dry eyes, dry mouth, dry skin, and muscle pain. Finally, promising new treatments are being studied. Scientists are working on ways to repair salivary glands that have been damaged and are developing an artificial salivary gland that can be implanted into the body. What Can I Do to Manage Dry Mouth? You can also try these other steps, which may help improve saliva flow: • Suck on sugar-free candy or chew sugar-free gum, specifically ones with xylitol. Try to avoid acidic ones like lemon that can soften teeth. Suck on ice chips or sugar-free ice pops. Never chew ice, since it can damage your teeth. These sucking and chewing actions help stimulate saliva flow. But also keep in mind that even though they don't have sugar, candies, ice pops, and gum may soften your teeth's enamel. To reduce the risk of cavities and tooth wear, use them only in moderation. • Drink plenty of water to help keep your mouth moist and loosen mucus. Carry water with you to sip throughout the day, and keep water by your bed at night. • Brush with a fluoride toothpaste, use a fluoride rinse, and visit your dentist regularly. Avoid commercial mouth rinses or mouthwashes that contain alcohol or peroxide. These ingredients will further dry out your mouth. • Breathe through your nose, not your mouth, as much as possible. • Use a room vaporizer to add moisture to bedroom air. • Use an over-the-counter artificial saliva substitute. • Moisten foods with broths, soups, sauces, gravy, creams, and butter or margarine. Eat soft, moist foods that are cool or at room temperature. • Avoid salty foods, dry foods (such as crackers, toast, cookies, dry breads, dry meats/poultry/fish, dried fruit, and bananas) and foods and beverages with high sugar content. • Avoid drinks with alcohol or caffeine (like coffees, teas, some colas, and chocolate-containing drinks). Alcohol increases water loss by triggering frequent urination. Alcohol, as well as caffeine, also dries out the mouth. Also avoid acidic beverages, such as any fruit juices (orange, apple, grape, grapefruit) and tomato juice. To ease irritation linked with dry mouth: • Limit spicy or salty foods, as these may cause pain in a dry mouth. • Quit smoking. • Use a moisturizer on your lips. • Use a soft-bristled toothbrush on your teeth and gums; rinse your mouth before and after meals with plain water or a mild mouth rinse (8 ounces of water, ½ teaspoon salt, and ½ teaspoon baking soda).

By 7001124384
•
October 25, 2023
Why Is the Holiday Season Bad for Your Teeth? There are a few reasons why dental health problems like tooth decay and gum disease are more common around the holidays: Sugary Sweets Galore Pumpkin pie, candy canes, and other holiday staples are chock-full of sugar. Overindulging in them attracts bacteria that produce acids that eat away at your tooth enamel, causing cavities. Grazing on Snacks Many of us spend Thanksgiving and Christmas catching up with loved ones while snacking throughout the day. Unfortunately, grazing doesn’t give your saliva a chance to clean the bacteria from your teeth after eating, which increases your risk of decay. Throwing Off Your Routine It’s easy for your normal oral hygiene routine to get thrown out of whack this time of year, especially if you’re traveling. Whether you forgot to pack your toothbrush or you stayed up too late with family and fell asleep without brushing, failing to clean your mouth as often as you typically do can lead to disaster. How to Protect Your Smile During the Holidays Just because it’s the holiday season doesn’t necessarily mean your oral health is doomed. There are plenty of things you can do to keep your smile safe: • Only eat at mealtimes – By reducing the number of times you eat per day, you give your teeth a better chance of protecting themselves from bacteria and acids. • Drink plenty of water – Water rinses lingering food particles off your teeth, preventing them from causing harm. • Brush and floss when you can – Remember to pack your toothbrush, toothpaste, and floss if you’re traveling. Also, set reminders to clean your teeth at least twice a day. • Limit hard, sticky, and sugary foods – Hard candies, caramel, gummy candies, and other seasonal sweets can all too easily damage your teeth. • Schedule a dental appointment – The end of the year is a great time to book your routine dental cleaning if it’s been more than six months. 770-304-0034 The holiday season is by far the worst time of year in terms of your dental health, but by keeping the tips above in mind, you can start the new year off on the right foot with a healthy smile! Author: Central Dental Associates, MA
By 7001124384
•
August 21, 2023
What a difference a Cleaning Makes Overtime, buildup accumulates on our teeth, especially near the gum line. And although it may not be visible when you smile in the mirror, through intraoral photos we’re able to see that buildup a lot clearer. The before photo on the left shows plaque that’s built-up at the gum line in just 6 months! That plaque contains millions of bacteria that eat away at your teeth and gums causing issues such as cavities and periodontal disease. Regular flossing, brushing, and dental visits help to ensure that your teeth maintain their healthy clean appearance as seen in the after photo.

By 7001124384
•
July 25, 2023
The aging mouth - and how to keep it younger Teeth, gums, and the rest of the oral cavity need extra care and attention if you want them to stay healthy in your later years. Aging isn't always pretty, and your mouth is no exception. (Ever consider why you shouldn't look a gift horse in the mouth?) A century ago the need for dentures in later life was almost a foregone conclusion. Today, three-quarters of people over 65 retain at least some of their natural teeth, but older people still suffer higher rates of gum disease, dental decay, oral cancer, mouth infections, and tooth loss. While these problems are nothing to smile about, you can still do a lot to keep your mouth looking and feeling younger than its years. Wear and tear Teeth are amazingly strong. Your molars can bear down with over 200 pounds of pressure. But they're not indestructible. A lifetime of crunching, gnawing, and grinding wears away the outer layer of enamel and flattens the biting edges. Tooth surfaces are also affected by exposure to acidic foods such as citrus fruits and carbonated beverages, which dissolve the protective enamel. Weakened enamel can set the stage for more serious dental problems. A crack or break in the tooth's outer surface leaves the delicate pulp tissue vulnerable to irritation and inflammation. And, since the nerves at the tooth's core lose sensitivity with age, the problem may be well advanced before you notice any pain. If an infection develops, you could need a root canal procedure or even lose the tooth entirely. The chance of having tooth damage severe enough to require a root canal or similarly invasive procedure triples once you're over age 65. The consolation prize: reduced nerve sensitivity means that procedures that may have been uncomfortable for younger people could hurt less if you are older. Just because you've got a few gray hairs doesn't mean you're out of the woods when it comes to cavities, either. The rate of tooth decay in people over 65 now outpaces that of schoolchildren. A prime target of dental caries in older adults is around the neck of the tooth, adjacent to the gum line. Gum tissue naturally recedes with age, so the soft root tissue becomes exposed. In addition, adults who grew up before the advent of fluoride products and dental sealants often have fillings from childhood and adolescence that eventually break down. Decay around the edges of those fillings is also a problem. While there's not much you can do to stem the natural attrition of the tooth surface, the pillars of cavity prevention — brushing, flossing, and regular cleanings at the dentist's office — remain the same at any age. People who have trouble brushing and flossing by hand because of arthritis or other disabilities should probably switch to an electric toothbrush. Fluoride, found in toothpaste, mouth rinses, and tap water in some communities, helps the body rebuild the mineral crystals that make up the tooth enamel and may also inhibit bacteria-laden plaque from adhering to the teeth. Fluoride rinses and gels, and varnishes applied by a dentist, may be able to halt the progression of root decay and in some cases reverse the damage. Article written by Harvard Health Publishing (2010)

By 7001124384
•
May 24, 2023
Say Ahhhh – What Your Tongue Can Tell You About Your Health Our tongue, it’s one of those things we all take for granted! As children we explored the world with our tongues, licking everything in sight (much to our mother’s dismay) and sticking it out at our siblings and parents just to get their reaction. As young adults we learned there was more to our tongue while exploring our first kisses and exotic foods. But the tongue is more than just a random body part, our tongues play a key role in our ability to taste and swallow food. And believe it or not, your tongue can also provide your dentist with clues to both your oral health and your overall health. In fact, you might be surprised what your tongue can tell you about your health. Get ready to say, “Ahhhhhhh!” What Your Tongue Can Tell You About Your Health White Coating on Tongue Your tongue is supposed to be a lovely shade of pink. If parts of your tongue appear to be coated with a white substance, this could be oral thrush, a yeast overgrowth that occurs inside the oral cavity. Of course, it could just be whitish from not brushing your tongue every time you brush your teeth. You do that, don’t you? If the white brushes away, you’re good to go. White Patches on Tongue Leukoplakia is a condition that can happen if the tongue has been irritated, such as with smoking or tobacco use. Every medical professional will advise you to quit that tobacco habit, but it’s ultimately up to you. If you see white patches, though, book a dentist appointment to be on the safe side and to rule out oral cancer. Overly Red Tongue While an overly red tongue can be a symptom of a Kawasaki disease, it’s much more commonly associated with a vitamin deficiency, such as folic acid or B-12. The solution could be simply adding a vitamin supplement to your morning smoothie. That’s not so bad, right? Irregular Red Bumpy Patches If your tongue looks like a roughly drawn map of irregular red and bumpy patches, this isn’t a fortune-teller sign that you’ll be going on a trip soon. You might be suffering from a high fever, in which case, taking a long journey overseas is the last thing you should be doing! Tender, Sore Tongue If your tongue is overly sensitive in one spot or all over, you could have a food allergy or a developing canker sore. Don’t worry about it, unless it doesn’t go away for a time. After that, time to call in the dentist for a professional opinion! Hairy Tongue Yep, sounds strange, but sometimes a protein build-up can cause small bumps to become elongated trapping food resulting in what looks like strands of hair on your tongue. Usually a good brushing or tongue scraping will take care of it, but if it doesn’t, a trip to the dentist is in order. Your dentist is the first line of defense against both serious and benign health concerns. So, stick out your tongue at the dentist and be ready for a comprehensive oral checkup. You never know what your tongue might be telling you about your health! Worried about your tongue or just need to schedule a dental check-up? We look forward to seeing you and seeing what that tongue of yours is telling us about your health. Reviewed by Aurora Dentist Dr. Lei Fu, general dentist at PERFECT TEETH – Green Valley Ranch.
VISIT US
,
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
HOURS
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
We Are Now Open One Friday Every Month From 8am-1pm:
Jan. 26, 2024 • Feb. 16, 2024 • March 15, 2024
April 12, 2024 • May 17, 2024 • June 21, 2024
Aug. 23, 2024 • Sept. 6, 2024 • Oct. 18, 2024
Nov. 15, 2024 • Dec. 13th & 20th, 2024
CONTACT US
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Hi. Do you need any help?
Privacy Policy
| Do Not Share My Information
| Conditions of Use
| Notice and Take Down Policy
| Website Accessibility Policy
© 2024
The content on this website is owned by us and our licensors. Do not copy any content (including images) without our consent.


Share On: